What Is Pimple on the Face? Causes, Types & Effective Treatments
- Home
- Acne Scars
- What Is Pimple on Face?

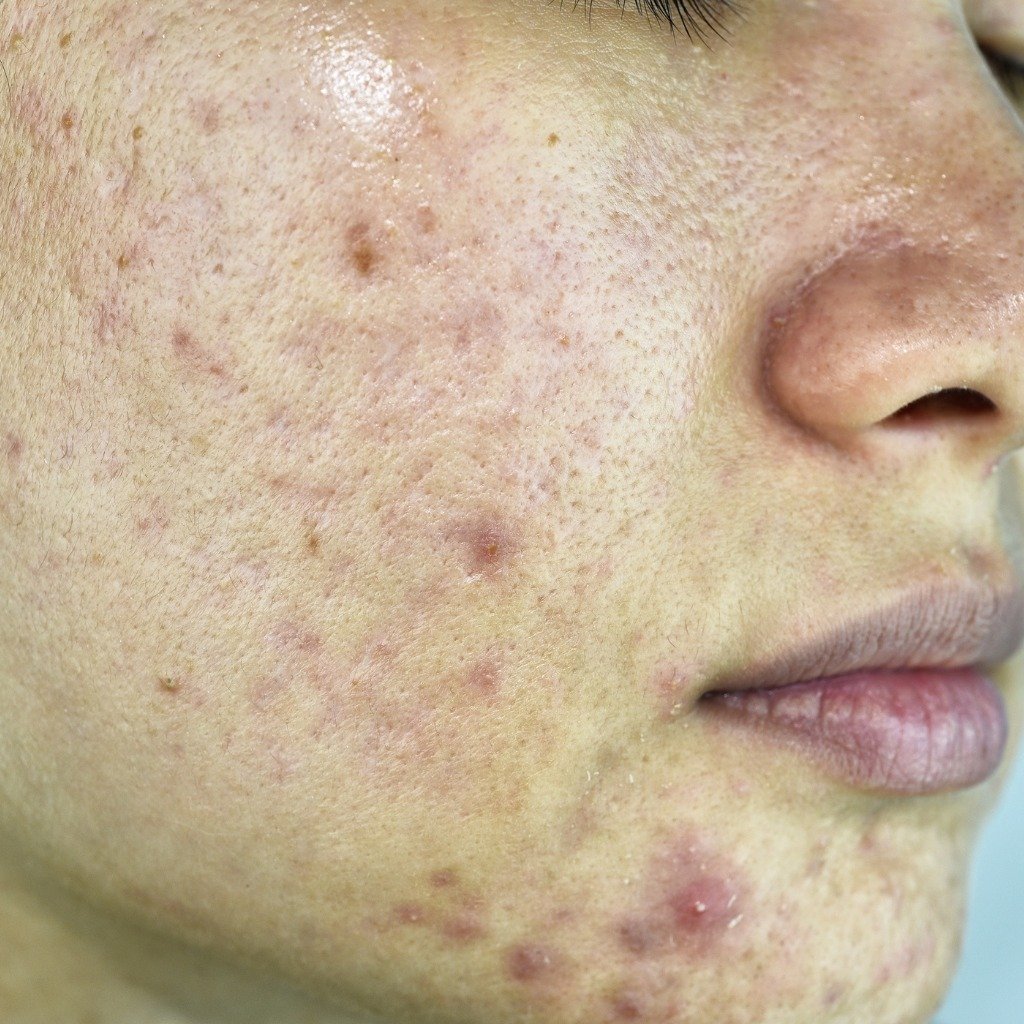
A pimple on the face, sometimes called acne, begins when hair follicles become clogged by excess oil (sebum), bacteria and dead skin cells. This clogging can lead to non‑inflammatory lesions such as blackheads and whiteheads or to inflammatory lesions like papules, pustules and cysts. Understanding what a pimple and acne come down to knowing how this clogging occurs and why.
The process starts in the sebaceous glands that lubricate the skin. When these glands produce too much oil, it mixes with dead skin cells and debris and forms plugs that block the follicle openings. This blockage creates an ideal environment for the growth of Propionibacterium acnes (now called Cutibacterium acnes). Once bacteria invade the clogged follicles, they break down sebum into inflammatory substances. The immune system responds by sending white blood cells to fight the infection, resulting in the redness, swelling and pus that typify pimples.
You might wonder if a pimple is a spot? Yes—both terms refer to localised clogged follicles. Curious about what a big pimple looks like? A severe inflammatory response can produce large, painful cysts or nodules; these lesions may cause scarring if not treated promptly. Similarly, pimple size depends on how deeply the follicle is blocked and how strong the inflammatory response is. What determines pimple size often comes down to how much sebum and bacteria are trapped in the pore. Effective pimple prevention treatment and strategies aim to minimise these blockages and control inflammation early.
What Role Does Oil Production Play in Acne?
Excessive oil production is a key driver of acne. The sebaceous glands are vital for skin hydration and protection, yet when they produce too much oil, the sebum combines with dead skin and traps bacteria. This combination clogs pores, creating a breeding ground for bacteria and leading to acne vulgaris.
Dermatologists often recommend products containing salicylic acid or benzoyl peroxide to control sebum output. These agents unclog pores and reduce bacterial growth. Maintaining balanced oil production helps prevent the formation of both small whiteheads and large, painful pimples.
Factor | Role in Acne Formation |
Excess Oil | Clogs pores and traps bacteria |
Dead Skin Cells | Combine with oil to block pores |
Bacteria | Thrive in blocked, oily environments |
Treatments | Aim to reduce oil, clear pores and kill bacteria |

Can Hormonal Changes Cause Breakouts?
Many people ask why they have pimples if they cleanse regularly. Hormonal fluctuations are often the answer. During puberty, menstrual cycles, pregnancy or conditions like polycystic ovary syndrome (PCOS), the body produces more androgens (e.g., testosterone). Higher androgen levels stimulate sebaceous glands to produce more oil, which can cause pores to clog and pimples to form. Teenagers and young adults experience this form of hormonal acne more often, but adults can also be affected.
To manage hormonal acne, treatments such as topical retinoids, oral contraceptives (for women) and anti‑androgen medications may be prescribed. These medical options fall under the broader category of hormonal acne treatment. Lifestyle modifications—balanced diet, regular exercise and stress management—also help stabilise hormone levels. Using non‑comedogenic skincare products and reducing mechanical friction (e.g., tight helmets or masks) can further limit acne mechanica flare‑ups.
How to Prevent Acne on Your Face?
Preventing acne involves a combination of home remedies, dietary adjustments, and consistent skincare practices. Research shows that certain natural ingredients reduce inflammation and bacteria, while low‑glycemic diets and gentle cleansing routines decrease breakout frequency and severity.
How Can Diet Impact Acne?
While topical remedies manage surface symptoms, dietary changes can influence internal inflammation and hormone levels. Certain foods may worsen acne:
|
Foods to Limit |
Reason |
|
High-glycemic index foods |
Increase blood sugar and insulin, driving sebum production and inflammation |
|
Dairy products |
Hormonal components may exacerbate acne, particularly skim milk |
|
Fast food |
Often high in fats and sugars, which promote inflammatory responses |
Conversely, foods rich in omega‑3 fatty acids, antioxidants and zinc can help soothe inflammation and support clear skin. While diet alone may not cure severe acne, making mindful food choices can complement medical treatment.
What Skincare Practices Help Reduce Pimples?
A targeted skincare regimen is essential:
- Regular cleansing: Use a gentle, non‑stripping cleanser twice daily to remove impurities without irritating the skin.
- Exfoliation with salicylic acid: This helps dissolve the bonds between dead skin cells, preventing clogged pores and reducing how pimples look and feel of pimples.
- Professional guidance: Consult a dermatologist for personalised advice and evidence‑based treatments. They can help you decide when a pimple is just a spot and when it’s part of more complex acne requiring prescription therapy.

Types of Acne and How to Identify Them
Acne manifests in various forms, each with distinct characteristics and severity. Recognising different types helps tailor treatment.
What Are Whiteheads and Blackheads?
Whiteheads (closed comedones) and blackheads (open comedones) are the most common non‑inflammatory forms of acne. Whiteheads occur when pores remain closed at the surface, trapping sebum and dead skin cells beneath. Blackheads form when the pore is open, allowing oxidation that darkens the plug. These lesions often appear on the nose, chin and forehead—areas with more sebaceous glands. Frequent, gentle cleansing and exfoliation can help manage them.
How to Recognise Cystic Acne
Cystic acne is a severe, inflammatory type characterised by deep, painful nodules or cysts under the skin. These lesions are large, red and tender, often lingering for weeks and leaving scars if untreated. They develop when a combination of bacteria, oil and dead skin cells becomes trapped deep in the pores, triggering an intense immune response. People with recurring deep, painful breakouts should seek professional help promptly.
What Is Acne Vulgaris?
Acne vulgaris encompasses multiple forms of acne:
- Comedonal acne: Includes whiteheads and blackheads caused by clogged follicles.
- Papulopustular acne: Involves small, red papules and pus‑filled pustules—the classic “pimple” look.
- Nodular and cystic acne: Severe forms presenting as large, painful lumps beneath the surface.
Factors such as genetics, hormones, and the environment influence the type of development. Knowing the kind helps determine appropriate treatments.
Understanding the Face Map and Acne
Face mapping is an ancient diagnostic practice suggesting that acne location reflects internal health. Some modern studies explore correlations between acne distribution and underlying issues, though evidence remains inconclusive.
What Does Acne Location Indicate?
Traditional face maps link areas of the face to specific internal organs:
- Forehead: Breakouts may correspond to digestive stress or poor diet, sometimes hinting at liver overload or irregular sleep.
- Cheeks: Acne here may be influenced by respiratory issues, pollution, allergies, smoking or contact with dirty surfaces (e.g., phone screens).
- Chin and jawline: Often associated with hormonal imbalances connected to reproductive organs; breakouts here are common during menstrual cycles or PCOS.
Viewing acne as a potential symptom of systemic imbalance encourages a holistic approach to treatment. However, face mapping should complement, not replace, evidence‑based dermatology.
How Can a Face Map Help in Treatment?
By observing patterns on a face map, dermatologists may adjust treatments. For instance, persistent forehead acne could prompt discussions about diet, while jawline breakouts might lead to hormonal evaluations and hormone‑regulating therapies. While face mapping is not scientifically proven, it can guide deeper health investigations and personalised care plans.

Management and Treatment of Acne
Effectively managing acne requires understanding when to seek professional care and which treatments suit your condition.
When to See a Dermatologist?
Seek a dermatologist if acne persists despite over‑the‑counter products or if you experience severe symptoms such as deep cysts, widespread nodules or potential scarring. A dermatologist can differentiate acne from other conditions and develop an individualised plan. Early intervention reduces scarring and ensures that misconceptions—such as equating facial pimples with unrelated conditions—are corrected.
What Are Common Treatment Options?
Treatment options span topical medications, oral prescriptions and in‑clinic procedures:
Treatment Type | Common Examples |
Topical treatments | Benzoyl peroxide, retinoids, salicylic acid |
Oral medications | Antibiotics, hormonal contraceptives, anti-androgen agents |
Dermatological procedures | Chemical peels, laser therapy, light therapy, drainage/extraction |
Topical treatments reduce inflammation, unclog pores and prevent new pimples. Oral medications address systemic factors like bacterial overgrowth or hormonal imbalances. Advanced procedures can diminish scarring or target severe cystic acne. A personalised combination often yields the best results.
Conclusion
Acne is a multifactorial dermatological condition shaped by genetic, hormonal and environmental factors. It arises from overactive oil glands, clogged follicles, bacterial proliferation and inflammatory responses. Understanding how pimples are formed on the face and what they look like helps individuals choose appropriate prevention and treatment strategies.
While face mapping offers an interesting perspective, evidence‑based approaches—correctly identifying acne types, adhering to preventive measures, and using tailored treatments—remain the foundation of clear‑skin management. Ongoing research continues to refine our knowledge of acne’s pathophysiology and improve therapies.






Сфера недропользования — это совокупность процессов, связанный с изучением и использованием недр.
Оно включает добычу полезных ископаемых и их промышленное освоение.
Недропользование регулируется законодательством, направленными на безопасность работ.
Грамотный подход в недропользовании способствует экономическому росту.
оэрн
Гедонизм — это направление в философии, которое ставит удовольствие в центр человеческой жизни.
Согласно этому взгляду, поиск радости считается важным мотивом существования.
Данная философия не всегда подразумевает отсутствие ограничений.
Во многих трактовках он предполагает баланс и контроль желаний.
https://telegra.ph/Rick-Owens-12-25
Современное понимание гедонизма часто акцентирует внимание на внутреннем комфорте.
При этом важную роль играет баланс между удовольствиями и реальными возможностями.
Гедонистический подход может поддерживать психологическое равновесие.
В целом, гедонизм рассматривается как философская перспектива, а не как отказ от ответственности.
нейросеть студент бот нейросеть студент бот .
нейросеть реферат онлайн нейросеть реферат онлайн .
нейросеть для студентов онлайн нейросеть для студентов онлайн .
нейросети для студентов нейросети для студентов .
нейросеть реферат нейросеть реферат .
нейросеть студент бот нейросеть студент бот .
водопонижение иглофильтрами грунтовых вод xn—77-eddkgagrc5cdhbap.xn--p1ai .
устройство водопонижения xn—77-eddkgagrc5cdhbap.xn--p1ai .
водопонижение строительных котлованов водопонижение строительных котлованов .
mostbet пополнить счет 2026 https://mostbet61527.help/
водопонижение строительное xn—77-eddkgagrc5cdhbap.xn--p1ai .
водопонижение на строительной площадке xn—77-eddkgagrc5cdhbap.xn--p1ai .
мостбет блэкджек https://mostbet61527.help/
best sms activation services github.com/SMS-Activate-Alternatives .
мостбет рабочий сайт Кыргызстан https://mostbet61527.help
проект водопонижения xn—77-eddkgagrc5cdhbap.xn--p1ai .
best sms activation services github.com/SMS-Activate-Alternatives .
mostbet надежность https://mostbet61527.help
sms activate sms activate .
mostbet быстрые ставки mostbet быстрые ставки
mostbet фрибет Кыргызстан mostbet фрибет Кыргызстан